Established 2005 Registered Charity No. 1110656
Scottish Charity Register No. SC043760
DONATE
Please help us to help more homeless people by setting up a monthly direct debit.
the Pavement relies on donations and volunteering from individuals and companies...
MORE ON DONATING
RECENT TWEETS
A new set of guidelines have been produced to help homeless people being released from hospital
The Pavement has previously noted how important it is that rough sleepers take care of their health. As they live in temporary or insecure accommodation, they are more vulnerable than the rest of the population. They may have difficulty in accessing primary care, and often do not seek treatment until the problem is at an advanced stage. Hospitals and medical staff cannot always understand rough sleepers - they may discharge themselves because of anxiety about losing their already temporary accommodation; "home" will not include the care and treatment that patients should receive.
Guidelines released only a few months ago aim to solve a problem obvious in the following cases. Bart, who is in his mid-30s, arrived at the Broadway centre by ambulance with the line from a drip still in his arm. He had receiving emergency medical care for several weeks, but the hospital had declared him "fit for discharge". Bart explained he had nowhere to go: he was homeless. Staff had heard of the Broadway Centre, so brought him there, but it does not provide emergency housing and offers limited, basic medical services. Centre staff received no advance warning from the hospital, and as a result there was no bed in the hospital or in the Broadway centre for Bart, who had only a small plastic bag of belongings and wore clothes inappropriate for the weather. He had no medication, only a letter from the GP. Bart looked like he was going to have to sleep on the streets that evening and drastic action was needed. The Centre threatened to return Bart by taxi if the hospital did not collect him. After much discussion, the hospital sent someone to collect him, thanks, in part, to the staff's persistence.
Mary, 35, also used the services of the Broadway centre when she was discharged by the hospital where she had been treated for deep vein thrombosis (a result of prolonged drug use), which could have led to the amputation of her leg.
As these are not the only cases of rough sleepers needing special treatment, last December the Department for Health and the Department for Communities and Local Government (DCLG) issued a new set of guidelines produced in conjunction with Homeless Link (the national membership organisation for frontline homelessness agencies in England) and the London Network for Nurses and Midwives (LNNM). The guidelines - Hospital Admission and Discharge: People who are homeless or living in temporary or insecure accommodation - are aimed at health professionals and primary care providers to help them establish an effective hospital admission and discharge policy.
The document gives background information about homelessness and highlights, among other facts, that rough sleepers often self discharge for reasons such as ongoing or unrecognised mental health problems or alcohol/drug dependence. The document mentions nine steps which should be considered in developing a protocol, and recommends identifiying relevant organizations such as social services and voluntary agencies.
According to the guidelines, "[a] street outreach team or primary health or mental health team may have a keyworker, who can provide background information and support to the patient both during admission and following discharge. Identification of a patient's housing status, keyworking arrangements and special vulnerabilities at an early stage in the admission is vital to achieve an appropriately planned and timely discharge." The introduction stresses that "a better integrated health system can can help prevent or reduce homelessness. Previous documents also emphasise the need to change systems to be more responsive to patient's needs."
Early discharge of patients can only result in deteriorating patient health. The health services face the cost of treating the same patient over and over again, as Homeless Link executive Jenny Edwards pointed. Natalie Warman, of the LNNM, believes that these guidelines will begin to improve the quality of services delivered to the homeless, just as previous strategies have improved care to other vulnerable groups such as older people and children. According to Mrs Warnman, the feedback from colleagues has been encouraging.
But Alice Evans, head of policy analysis at Homeless Link, who was closely involved in drafting the guidelines, said: "it is too early to assess the level of improvement since the introduction of the hospital discharge guidelines for working with homeless patients. Our member groups - who've had to deal with past problems - are all pleased with the new guidelines. They are our eyes and ears, the ones who can best gauge the improvements."
The Pavement has previously noted how important it is that rough sleepers take care of their health. As they live in temporary or insecure accommodation, they are more vulnerable than the rest of the population. They may have difficulty in accessing primary care, and often do not seek treatment until the problem is at an advanced stage. Hospitals and medical staff cannot always understand rough sleepers - they may discharge themselves because of anxiety about losing their already temporary accommodation; "home" will not include the care and treatment that patients should receive.
Guidelines released only a few months ago aim to solve a problem obvious in the following cases. Bart, who is in his mid-30s, arrived at the Broadway centre by ambulance with the line from a drip still in his arm. He had receiving emergency medical care for several weeks, but the hospital had declared him "fit for discharge". Bart explained he had nowhere to go: he was homeless. Staff had heard of the Broadway Centre, so brought him there, but it does not provide emergency housing and offers limited, basic medical services. Centre staff received no advance warning from the hospital, and as a result there was no bed in the hospital or in the Broadway centre for Bart, who had only a small plastic bag of belongings and wore clothes inappropriate for the weather. He had no medication, only a letter from the GP. Bart looked like he was going to have to sleep on the streets that evening and drastic action was needed. The Centre threatened to return Bart by taxi if the hospital did not collect him. After much discussion, the hospital sent someone to collect him, thanks, in part, to the staff's persistence.
Mary, 35, also used the services of the Broadway centre when she was discharged by the hospital where she had been treated for deep vein thrombosis (a result of prolonged drug use), which could have led to the amputation of her leg.
As these are not the only cases of rough sleepers needing special treatment, last December the Department for Health and the Department for Communities and Local Government (DCLG) issued a new set of guidelines produced in conjunction with Homeless Link (the national membership organisation for frontline homelessness agencies in England) and the London Network for Nurses and Midwives (LNNM). The guidelines - Hospital Admission and Discharge: People who are homeless or living in temporary or insecure accommodation - are aimed at health professionals and primary care providers to help them establish an effective hospital admission and discharge policy.
The document gives background information about homelessness and highlights, among other facts, that rough sleepers often self discharge for reasons such as ongoing or unrecognised mental health problems or alcohol/drug dependence. The document mentions nine steps which should be considered in developing a protocol, and recommends identifiying relevant organizations such as social services and voluntary agencies.
According to the guidelines, "[a] street outreach team or primary health or mental health team may have a keyworker, who can provide background information and support to the patient both during admission and following discharge. Identification of a patient's housing status, keyworking arrangements and special vulnerabilities at an early stage in the admission is vital to achieve an appropriately planned and timely discharge." The introduction stresses that "a better integrated health system can can help prevent or reduce homelessness. Previous documents also emphasise the need to change systems to be more responsive to patient's needs."
Early discharge of patients can only result in deteriorating patient health. The health services face the cost of treating the same patient over and over again, as Homeless Link executive Jenny Edwards pointed. Natalie Warman, of the LNNM, believes that these guidelines will begin to improve the quality of services delivered to the homeless, just as previous strategies have improved care to other vulnerable groups such as older people and children. According to Mrs Warnman, the feedback from colleagues has been encouraging.
But Alice Evans, head of policy analysis at Homeless Link, who was closely involved in drafting the guidelines, said: "it is too early to assess the level of improvement since the introduction of the hospital discharge guidelines for working with homeless patients. Our member groups - who've had to deal with past problems - are all pleased with the new guidelines. They are our eyes and ears, the ones who can best gauge the improvements."
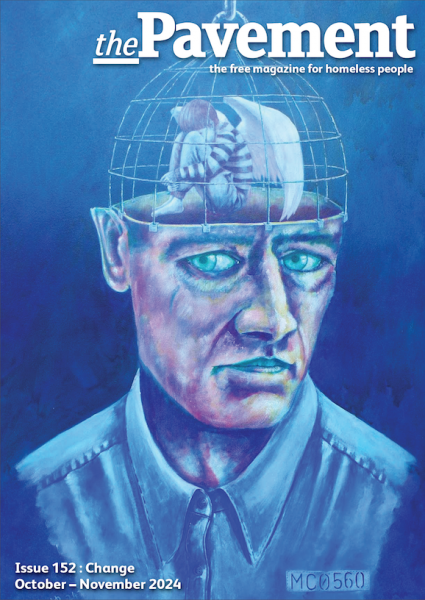
October – November 2024 : Change
CONTENTS
BACK ISSUES
- Issue 152 : October – November 2024 : Change
- Issue 151 : August – September 2024 : Being Heard
- Issue 150 : June – July 2024 : Reflections
- Issue 149 : April – May 2024 : Compassion
- Issue 148 : February – March 2024 : The little things
- Issue 147 : December 2023 – January 2024 : Next steps
- Issue 146 : October 2023 – November 2023 : Kind acts
- Issue 145 : August 2023 – September 2023 : Mental health
- Issue 144 : June 2023 – July 2023 : Community
- Issue 143 : April 2023 - May 2023 : Hope springs
- Issue 142 : February 2023 - March 2023 : New Beginnings
- Issue 141 : December 2022 - January 2023 : Winter Homeless
- Issue 140 : October - November 2022 : Resolve
- Issue 139 : August - September 2022 : Creativity
- Issue 138 : June - July 2022 : Practical advice
- Issue 137 : April - May 2022 : Connection
- Issue 136 : February - March 2022 : RESPECT
- Issue 135 : Dec 2021 - Jan 2022 : OPPORTUNITY
- Issue 134 : September-October 2021 : Losses and gains
- Issue 133 : July-August 2021 : Know Your Rights
- Issue 132 : May-June 2021 : Access to Healthcare
- Issue 131 : Mar-Apr 2021 : SOLUTIONS
- Issue 130 : Jan-Feb 2021 : CHANGE
- Issue 129 : Nov-Dec 2020 : UNBELIEVABLE
- Issue 128 : Sep-Oct 2020 : COPING
- Issue 127 : Jul-Aug 2020 : HOPE
- Issue 126 : Health & Wellbeing in a Crisis
- Issue 125 : Mar-Apr 2020 : MOVING ON
- Issue 124 : Jan-Feb 2020 : STREET FOOD
- Issue 123 : Nov-Dec 2019 : HOSTELS
- Issue 122 : Sep 2019 : DEATH ON THE STREETS
- Issue 121 : July-Aug 2019 : INVISIBLE YOUTH
- Issue 120 : May-June 2019 : RECOVERY
- Issue 119 : Mar-Apr 2019 : WELLBEING
- Issue 118 : Jan-Feb 2019 : WORKING HOMELESS
- Issue 117 : Nov-Dec 2018 : HER STORY
- Issue 116 : Sept-Oct 2018 : TOILET TALK
- Issue 115 : July-Aug 2018 : HIDDEN HOMELESS
- Issue 114 : May-Jun 2018 : REBUILD YOUR LIFE
- Issue 113 : Mar–Apr 2018 : REMEMBRANCE
- Issue 112 : Jan-Feb 2018
- Issue 111 : Nov-Dec 2017
- Issue 110 : Sept-Oct 2017
- Issue 109 : July-Aug 2017
- Issue 108 : Apr-May 2017
- Issue 107 : Feb-Mar 2017
- Issue 106 : Dec 2016 - Jan 2017
- Issue 105 : Oct-Nov 2016
- Issue 104 : Aug-Sept 2016
- Issue 103 : May-June 2016
- Issue 102 : Mar-Apr 2016
- Issue 101 : Jan-Feb 2016
- Issue 100 : Nov-Dec 2015
- Issue 99 : Sept-Oct 2015
- Issue 98 : July-Aug 2015
- Issue 97 : May-Jun 2015
- Issue 96 : April 2015 [Mini Issue]
- Issue 95 : March 2015
- Issue 94 : February 2015
- Issue 93 : December 2014
- Issue 92 : November 2014
- Issue 91 : October 2014
- Issue 90 : September 2014
- Issue 89 : July 2014
- Issue 88 : June 2014
- Issue 87 : May 2014
- Issue 86 : April 2014
- Issue 85 : March 2014
- Issue 84 : February 2014
- Issue 83 : December 2013
- Issue 82 : November 2013
- Issue 81 : October 2013
- Issue 80 : September 2013
- Issue 79 : June 2013
- Issue 78 : 78
- Issue 77 : 77
- Issue 76 : 76
- Issue 75 : 75
- Issue 74 : 74
- Issue 73 : 73
- Issue 72 : 72
- Issue 71 : 71
- Issue 70 : 70
- Issue 69 : 69
- Issue 68 : 68
- Issue 67 : 67
- Issue 66 : 66
- Issue 65 : 65
- Issue 64 : 64
- Issue 63 : 63
- Issue 62 : 62
- Issue 61 : 61
- Issue 60 : 60
- Issue 59 : 59
- Issue 58 : 58
- Issue 57 : 57
- Issue 56 : 56
- Issue 56 : 56
- Issue 55 : 55
- Issue 54 : 54
- Issue 53 : 53
- Issue 52 : 52
- Issue 51 : 51
- Issue 50 : 50
- Issue 49 : 49
- Issue 48 : 48
- Issue 47 : 47
- Issue 46 : 46
- Issue 45 : 45
- Issue 44 : 44
- Issue 43 : 43
- Issue 42 : 42
- Issue 5 : 05
- Issue 4 : 04
- Issue 2 : 02
- Issue 1 : 01
- Issue 41 : 41
- Issue 40 : 40
- Issue 39 : 39
- Issue 38 : 38
- Issue 37 : 37
- Issue 36 : 36
- Issue 35 : 35
- Issue 34 : 34
- Issue 33 : 33
- Issue 10 : 10
- Issue 9 : 09
- Issue 6 : 06
- Issue 3 : 03
- Issue 32 : 32
- Issue 31 : 31
- Issue 30 : 30
- Issue 29 : 29
- Issue 11 : 11
- Issue 12 : 12
- Issue 13 : 13
- Issue 14 : 14
- Issue 15 : 15
- Issue 16 : 16
- Issue 17 : 17
- Issue 18 : 18
- Issue 19 : 19
- Issue 20 : 20
- Issue 21 : 21
- Issue 22 : 22
- Issue 23 : 23
- Issue 24 : 24
- Issue 25 : 25
- Issue 8 : 08
- Issue 7 : 07
- Issue 26 : 26
- Issue 27 : 27
- Issue 28 : 28
- Issue 1 : 01